Medicare Fraud Whistleblower: Role, Protection, and Rewards
Medicaid and Medicare fraud comprises the largest area of fraud against the government today. An average of 10% of all medical bills in the United States are fraudulent or inflated. This fraud is why the Department of justice compensates large rewards to anyone who reports Medicare fraud.
Unfortunately, every dollar lost through Medicare medical fraud translates to one less dollar preserved for the elderly and challenged Americans needing health care. Everyone is therefore called upon to speak up about any Medicare fraud they may experience.
A whistleblower is a person, mostly an employee in a medical facility, who reveals information about activity in the facility, be it public or private, that is considered immoral, fraudulent, unsafe, illegal, or illicit.
Who Can Report Medicare Fraud?
Medicare fraud means a medical practitioner such as a doctor, hospice care provider, a nursing home, dentist, or hospital over-bills a patient. The typical frauds reported are billing for treatments that were never received or unnecessary procedures, tests that were never performed or were unnecessary, or bills for unnecessary equipment. Practices include upcoding and unbundling.
Many people believe that patients are the sole individuals who can report medical billing fraud. As much as patients are the subjects of fraud and should report when something goes wrong, the following category of people should also report Medicare fraud:
- Health facility administrators
- Pharmacists
- Doctors
- Nurses
- Hospital specialists
- Other employees
People working in a health facility have the inside knowledge of the right and the wrong way to treat patients and the billing process. The knowledge makes them ideal to perceive any malpractice in the hospital, particularly wrong bill reimbursement.
What Are the Ways to Report Medicare Fraud
The government is aware that reporting Medicare fraud is correct, but it is dangerous. The government has therefore provided a platform to report suspicious fraudulent medical behavior anonymously. There are two distinct ways to report such activities to the Inspector general or Medicare.
- Calling 1-800-HHS-TIPS or 1- 800-Medicare
- Online form submission
List of Items You Should Have Before You Report Medicare Fraud
- Your name and Medicare number
- Medical practitioner’s name and their ID number
- The service in question, prescription or treatment, and ID Number
- Date of service delivery, treatment, or product that was received or delivered
- Payment approved and paid for Medicare and Date
- Summary Notice (MSN)
- The reason why Medicare should not have refunded medical providers
- Any other report or evidence you have about why Medicare should not have paid
Medicare Fraud Whistleblower Compensation
Reporting Medicare fraud attracts up to a $1000 prize to qualified claims. However, there are five conditions for the reward to be paid.
- You must report a personal experience of Medicare fraud. The allegations must be specific and not generalized.
- Suspected Medicare fraud must be confirmed by the Medicare contractor responsible for investigating fraud as possible fraud. The issue must then be officially directed to the Office of the Inspector General for analysis.
- You must not have participated in the fraudulent act or are eligible for another claim reward for similar offenses.
- The health practitioner or organization must not be under investigation for the same offense as your allegation.
- Your report must result in a recovery of not less than $100.
Whichever is less, the should be equivalent to 10% of the recovered amount of $1,000. If the reward is eligible for more than one person, it should be shared among them.
| How to Report Medicare Fraud | |
| Medicare | Medicare Help Support |
| Whistleblower Claims | Whistleblower Info |
| The FBI | FBI Tips |
| The Centers for Medicare and Medicaid | CMS Support |
| US Health Department – Office of the Inspector General | OIG Complaints |
DoNotPay Will Easily Help You with Medicare Fraud Whistleblower Protection
Whistleblower cases are complex, especially when they fall under the False Claims Act. While fruitful cases can lead to considerable compensation by both the whistleblower and the government, some cases may be weak. However, you must not worry about how to make your case strong because we will help you with every step.
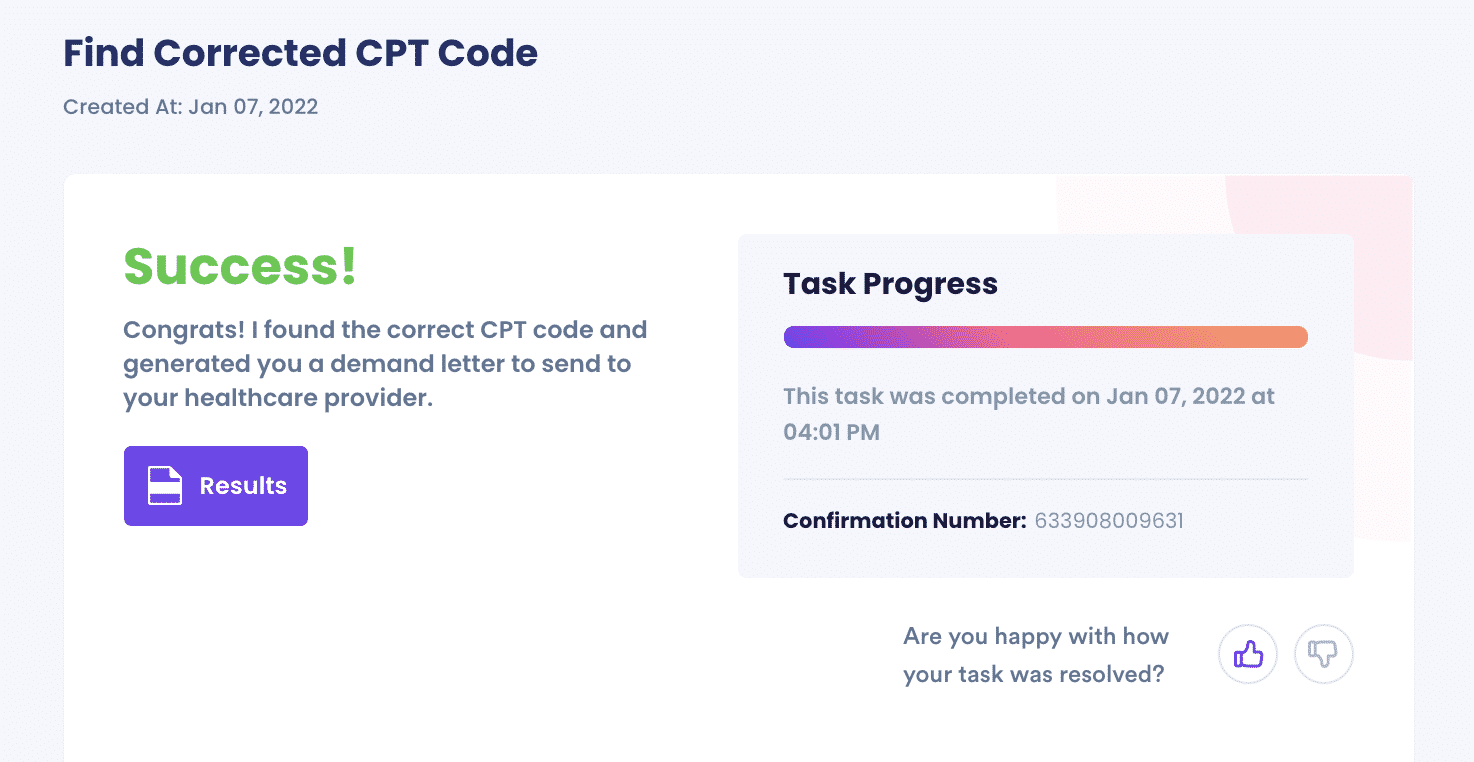
DoNotPay will help you report Medicare fraud from the comfort of your home through these steps:
- Search Fight Medical Fraud on DoNotPay.
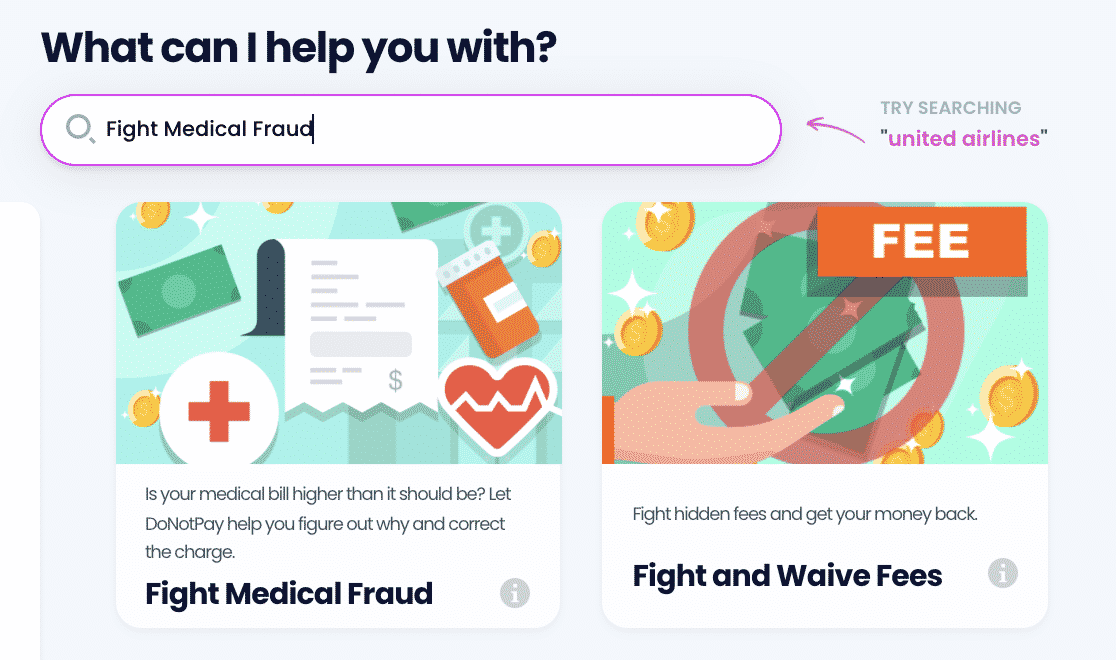
- Tell us the date of your visit, what you were treated for, and where you were treated.
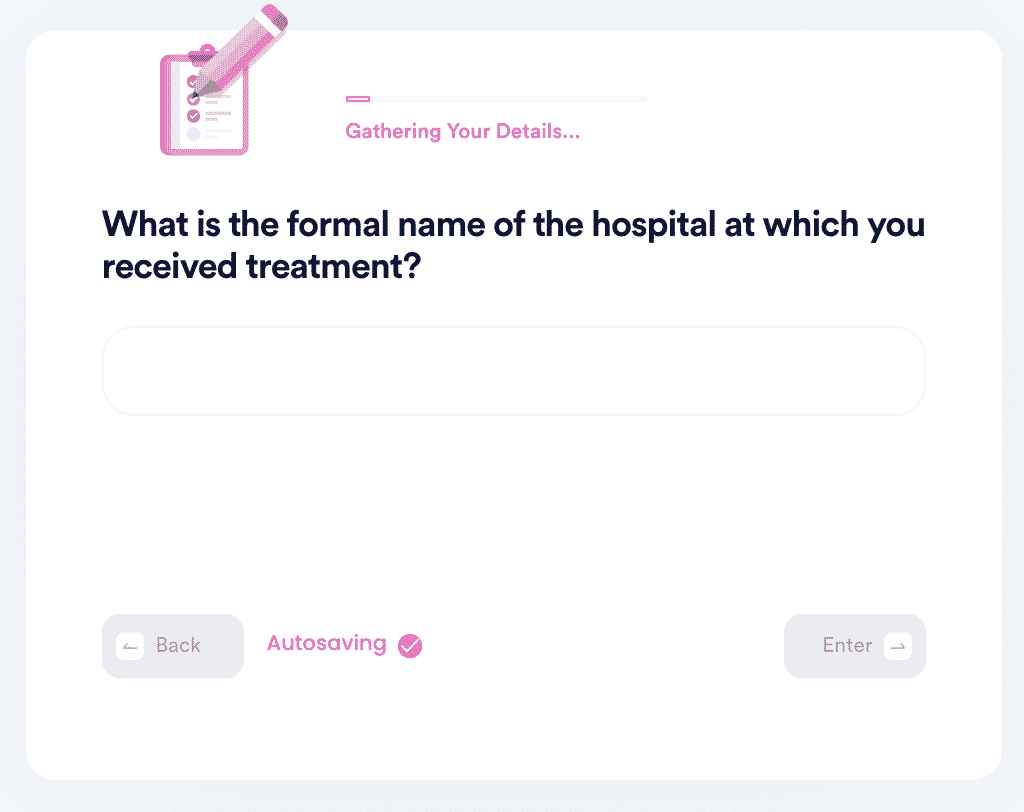
- Let us know what CPT code your visit was filed under. If you don’t know, we’ll generate a letter for you to send to your physician to request the code.
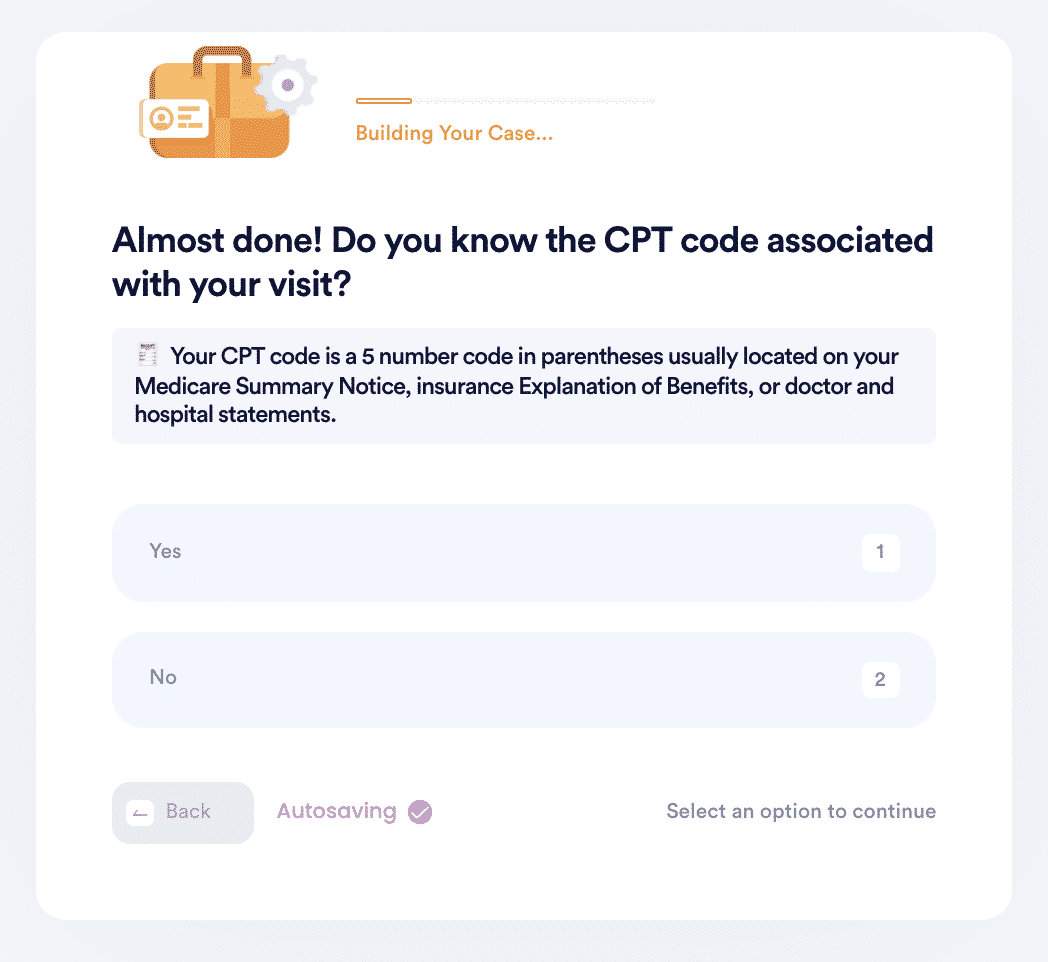
- Choose the correct CPT code or let us know if you want us to find it for you.
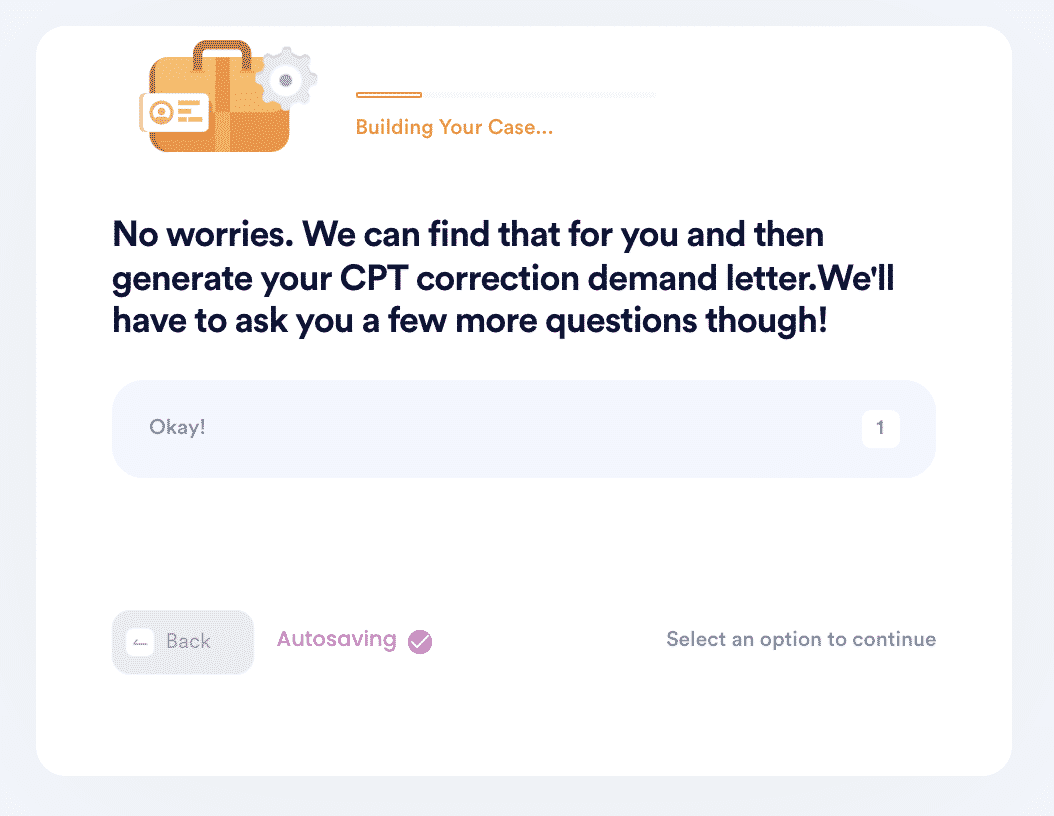
- And that’s it! DoNotPay will automatically find the correct CPT code for your visit if you don’t know it and then generate a demand letter on your behalf to send to your physician for a bill correction.
Report Healthcare Fraud Faster with the Help of DoNotPay
You should rely on DoNotPay to report healthcare fraud because it is a convenient service. You will not need to leave your home since you can access the service from the DoNotPay web browser or mobile app. The service is also faster. You will get a solution in a few minutes, unlike other cases where you have to wait for days before your case is handled.
Once you request to report Medicare fraud as a whistleblower using DoNotPay, rest assured that we shall present the case on your behalf, and you will get the best results.
Other Services You Can Get with DoNotPay
DoNotPay can help you detect upcoding and report fraud. Besides reporting Medicare fraud, DoNotPay can help with the following:
- Filing Complaints Against Companies
- Suing Others in Small Claims Court
- Creating Advance Healthcare Directives
- Requesting Sick Leave on Your Behalf
- Helping You Will Bills
Join DoNotPay today to find the correct CPT codes to your medical bills and demand corrections quickly!