How to Report Medicare Fraud and Get Your Bills Corrected
For every medical procedure including a checkup by your doctor, a laboratory test, x-ray, scan, surgery, etc. there is a current procedural terminology (CPT) code. These codes are assigned by the American Medical Association (AMA) and are copyrighted.
Why does this matter? When you have any form of medical test or care, the code is used to bill your insurance – for those 65 and older the code is used to bill Medicare and any other supplemental insurance you have. When improper coding is intentionally used, it is considered Medicare fraud. DoNotPay will help you or any fraudulent medical billing.
What Is CPT Upcoding and Unbundling?
Using CPT coding is customary for any medical office or facility and applicable to any form of medical insurance. Most doctor's offices have someone who specializes in medical billing. Hospitals employ multiple medical billers.
Sometimes mistakes are made. Codes may be entered improperly that have no relevance to the procedure. But when a medical facility intentionally uses a code that applies to a similar but more expensive procedure with the intent of making a few extra bucks, that is called upcoding and is problematic.
For example, say you had a simple one-view x-ray taken, but radiology billed out for two views. That is cheating, and more importantly, fraud. It can slip by Medicare or other insurance because a diagnosis was made based on the x-ray whether it was one view or two.
Unbundling Codes
Another form of medical billing fraud is unbundling. This is when multiple CPT codes are used for individual parts of a procedure to increase payment, rather than sampling billing for the procedure under its one CPT code.
The False Claims Act
Upcoding to Medicare is illegal under the False Claims Act enacted in 1863, following defense contractor fraud during the Civil War.
An Increase in Consumer Healthcare Expenses
Medicare upcoding increases health care costs which in turn is passed on to consumers like yourself through the cost of healthcare premiums and taxes.
How to Spot Medicare Fraud
As we get older, most of us tend to see doctors more often for a variety of ailments. In addition, we have more laboratory tests, x-rays, and other scans. Providers will first bill Medicare and will bill you for what Medicare does not cover.
You should carefully review your Medicare Summary Notice or Explanation of Benefits (EOB). This will explain what services and supplies have been billed, how much Medicare-approved for the service, and what Medicare has paid. In addition, it will reflect if and how much you may owe the provider.
As you review your summary check for:
- Billing from a physician or medical service you do not recognize
- Billing from a provider you know, but for a service, you did not receive
- Billing for service twice when you only had that service once
- Billing for a service that seems like upgrading, or upcoding, from what you had done
Any of these things are considered Medicare fraud and need to be reported.
How to Report Medicare Fraud on Your Own
If you suspect Medicare medical fraud, it is recommended that you contact the following:
| Office | Phone Number |
| Medicare | 1-800-MEDICARE (1-800-633-4227) |
| The U.S. Department of Health and Human Services – Office of the Inspector General | 1-800-368-1463 |
Be prepared to supply:
- Your name and your Medicare number, shown on your Medicare card
- The name, address, phone, and any other information you may have on the provider whom you are reporting
- The exact service and date of that service
- How much Medicare-approved and subsequently paid
- The date of the Medicare Summary Notice or EOB which you are referring to
To do this on your own requires time and patience. How about using an easier way?
How to Fight Medical Fraud and Get Your Bills Corrected
Using DoNotPay can make the process of reporting healthcare fraud so much easier. Not only will it write a demand letter for a bill correction to the fraudulent healthcare party, but if it does not get resolved to your satisfaction, you can use DoNotPay's Send demand letters to Now product to begin a small claims suit.
To have DoNotPay write your demand letter, just follow these five simple steps:
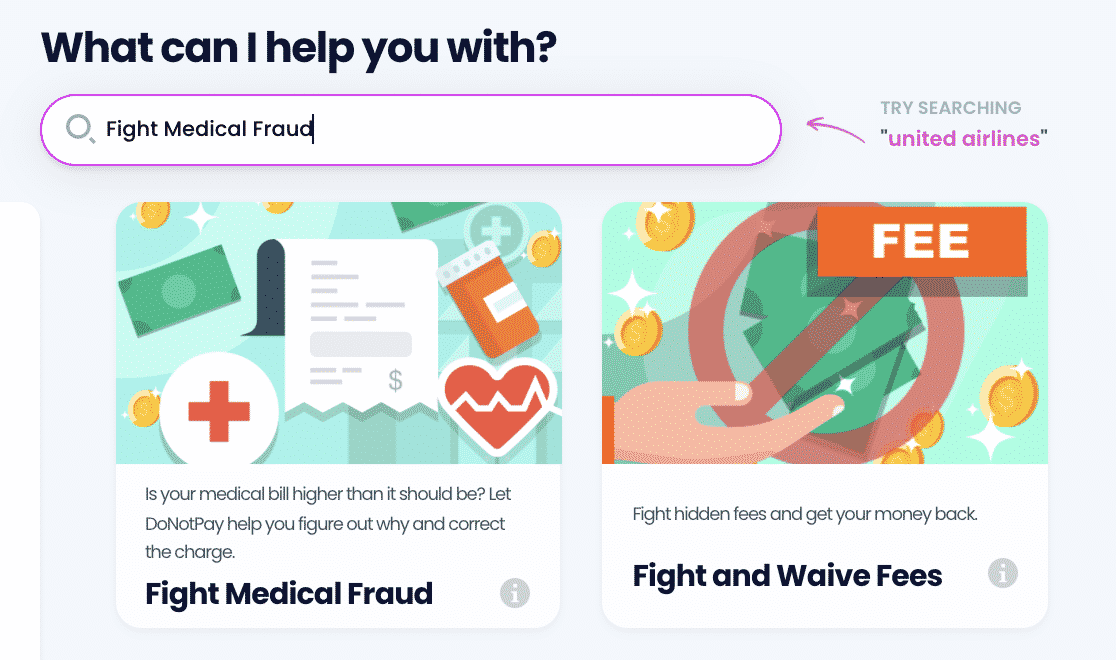
- Search Fight Medical Fraud on DoNotPay.
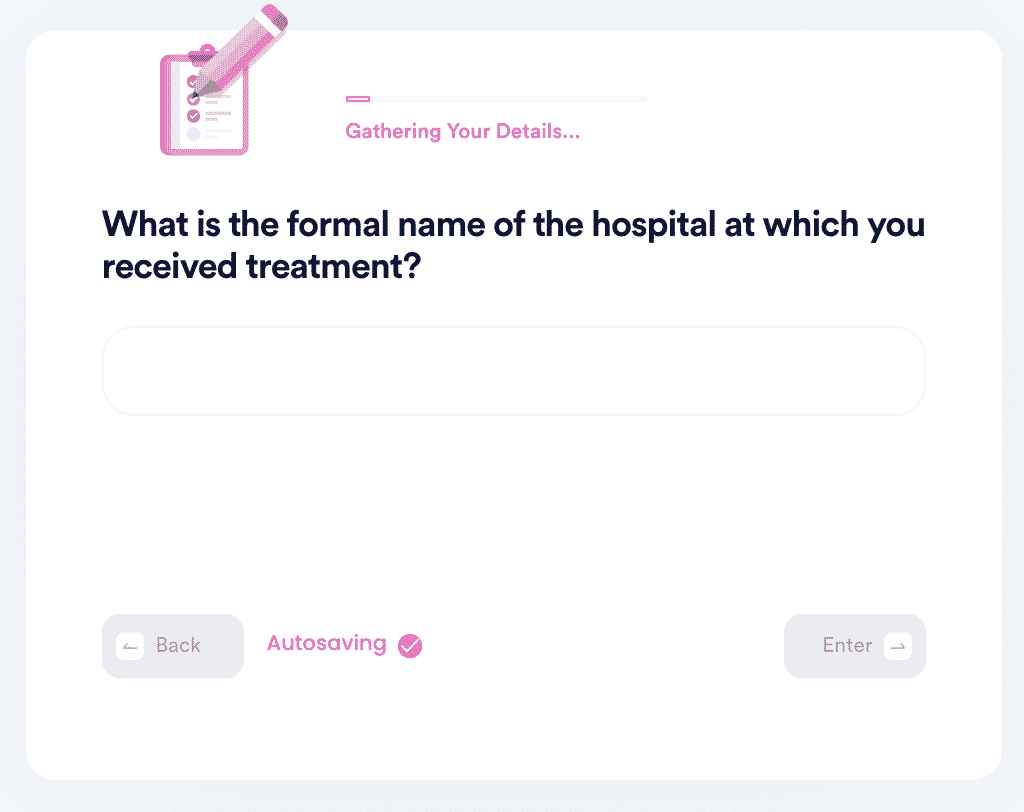
- Tell us the date of your visit, what you were treated for, and where you were treated.
- Let us know what CPT code your visit was filed under. If you don't know, we'll generate a letter for you to send to your physician to request the code.
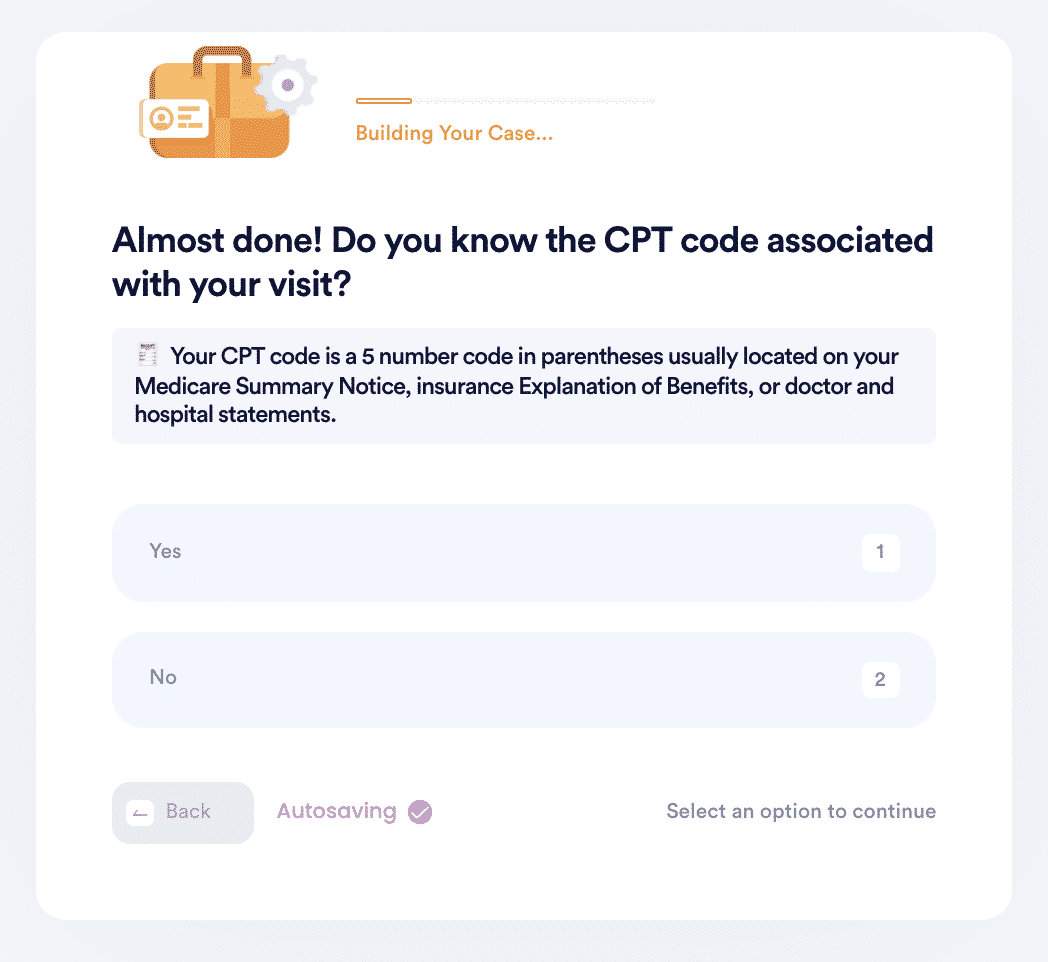
- Choose the correct CPT code or let us know if you want us to find it for you.
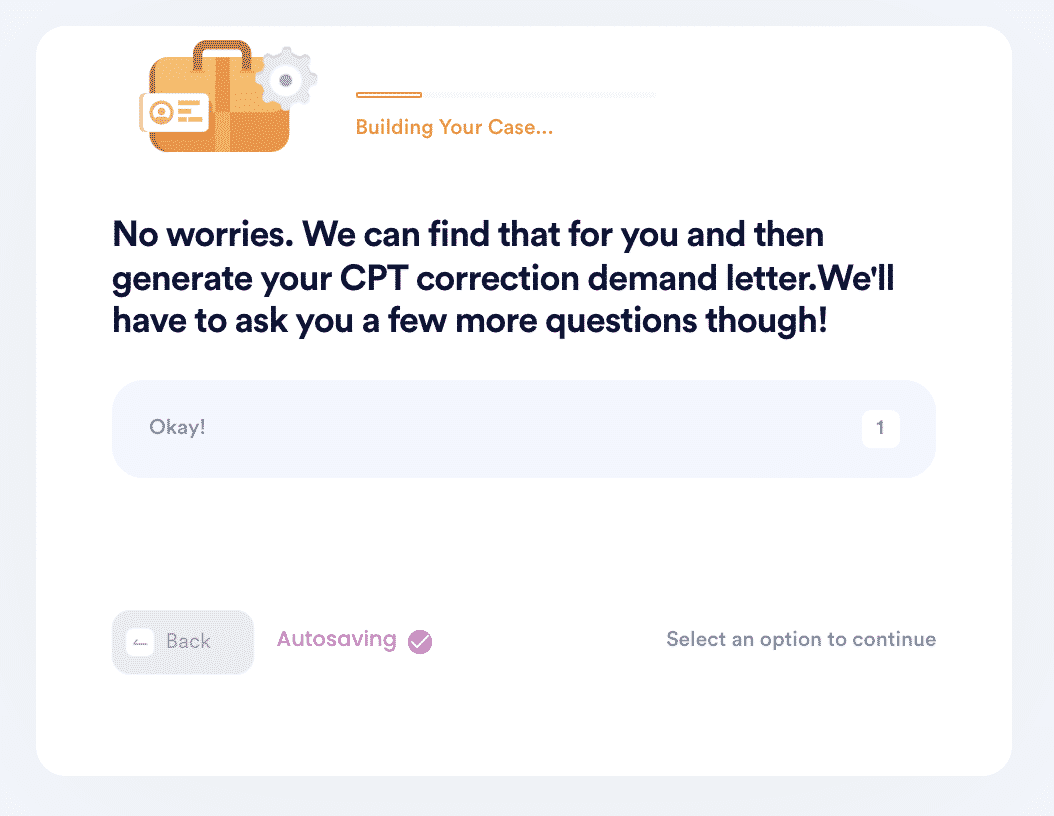
- And that's it! DoNotPay will automatically find the correct CPT code for your visit if you don't know it and then generate a demand letter on your behalf to send to your physician for a bill correction.
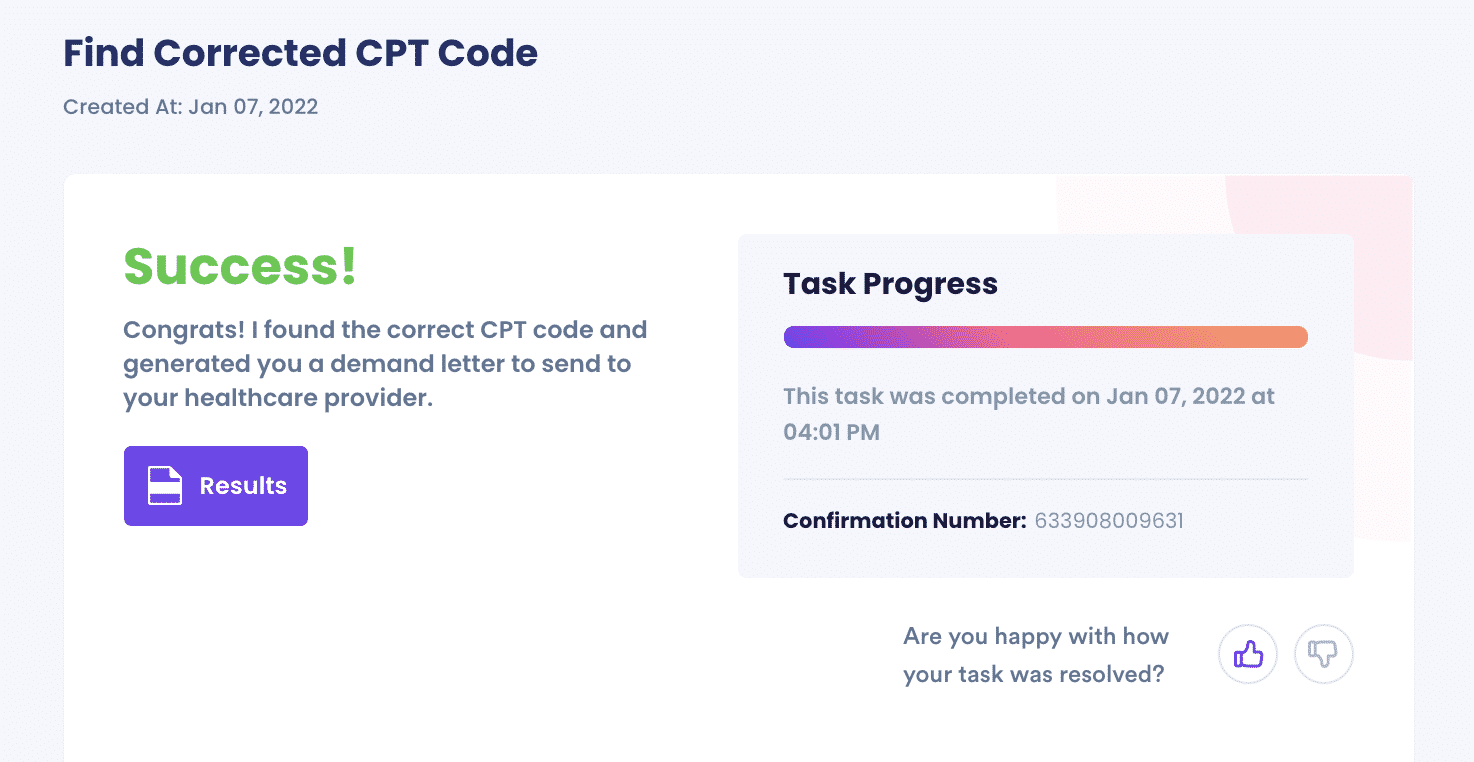
That is all there is to it. Now you just wait for a response. And while you are waiting, you can ask DoNotPay to take care of other issues for you.
Other Functions DoNotPay Provides
In addition to addressing the provider and , if you find you need to take the fraudulent healthcare billing facility to small claims court, DoNotPay will file the paperwork for you.
DoNotPay can also help you:
- Write your advance health care directive
- Write a request to your employer for sick leave
- Help you organize and pay your bills
- File a formal complaint with your local branch of government
When you have a look around on the DoNotPay site, you will see that there are a lot of issues it can help you with. Sign up now!
 By
By